Preparing for the Nov 1 changes to General Practice in Australia

General Practice is the backbone of the Australian health system, and on November 1, 2025, some of the most fundamental changes since the introduction of the Medicare program are set to take effect. These reforms, aimed at strengthening Medicare, improving patient access, and ensuring continuity of care, represent a significant administrative and financial adaptation for every GP and practice manager in the country.
It's understandable if your practice feels overwhelmed by the complexity of a new incentive program (BBPIP), expanded bulk-billing eligibility, and a complete overhaul of how mental health services are claimed. This transition is a heavy lift. The good news? It presents a critical opportunity to balance delivering high-quality, accessible care with improving the financial sustainability of your practice.
What GPs and Practice Managers need to know
The November 1, 2025, reforms primarily focus on strengthening Medicare by improving access to care and promoting continuity. GPs and Practice Managers need to focus on these three critical changes:
1. Expanded Bulk Billing Incentives (BBI) and the new BBPIP
Expanded BBI Eligibility
The existing Medicare Bulk Billing Incentive is being expanded to all Medicare-eligible patients, regardless of age or concession status. This is a significant uplift in the reward for bulk billing.
The Triple Incentive
GPs can claim the highest (triple) bulk billing incentive for bulk-billed face-to-face Levels B, C, D, and E general attendance consultations.
The Bulk Billing Practice Incentive Program (BBPIP) Commences
This is a new program offering an additional quarterly incentive payment of 12.5% of the MBS benefits earned for eligible services.
The Strict Requirement
To qualify for the BBPIP payment (which is split 50/50 between the doctor and the practice), the practice must commit to bulk billing every eligible service for every Medicare-eligible patient. Compliance is paramount.
2. Better Access (Mental Health) redesign
The structure for how GPs and Prescribed Medical Practitioners (PMPs) manage Mental Health Treatment Plans (MHTPs) is changing to improve continuity of care.
New Continuity Rules
Medicare benefits for the preparation of a MHTP (e.g., item 2715) and referrals will only be payable if the service is delivered by the GP or PMP at the patient's MyMedicare-registered practice or by the patient's usual medical practitioner.
Item Removal & New Claiming
Dedicated MHTP review items (e.g., 2712) and mental health consultation items are being removed. GPs and PMPs will now use the more flexible time-tiered professional (general attendance) MBS items for reviews and ongoing consultations. This requires robust, time-justified clinical documentation.
3. New opportunities for Long-Acting Reversible Contraception (LARC)
There are increased Medicare rebates for complex LARC services, including the insertion of an IUD (item 35503) and the implantation of hormonal implants (item 14206). This supports both patient access and practice revenue for women's health services.
How Lyrebird supports compliance & profitability
The November 1 reforms introduce a high-stakes environment where compliance with the BBPIP is essential and administrative efficiency is the key to financial sustainability. Lyrebird's AI medical scribe is uniquely positioned to handle these new demands, allowing your GPs to focus on patient care and your practice managers to secure revenue.
1. Maximising revenue through MBS item compliance
The BBPIP requires 100% compliance (bulk billing every eligible service), and the expanded BBI means selecting the highest-value triple incentive item is critical for profitability. Billing the wrong item, or accidentally charging a fee for an eligible service, can jeopardise the BBPIP payment.
How Lyrebird helps
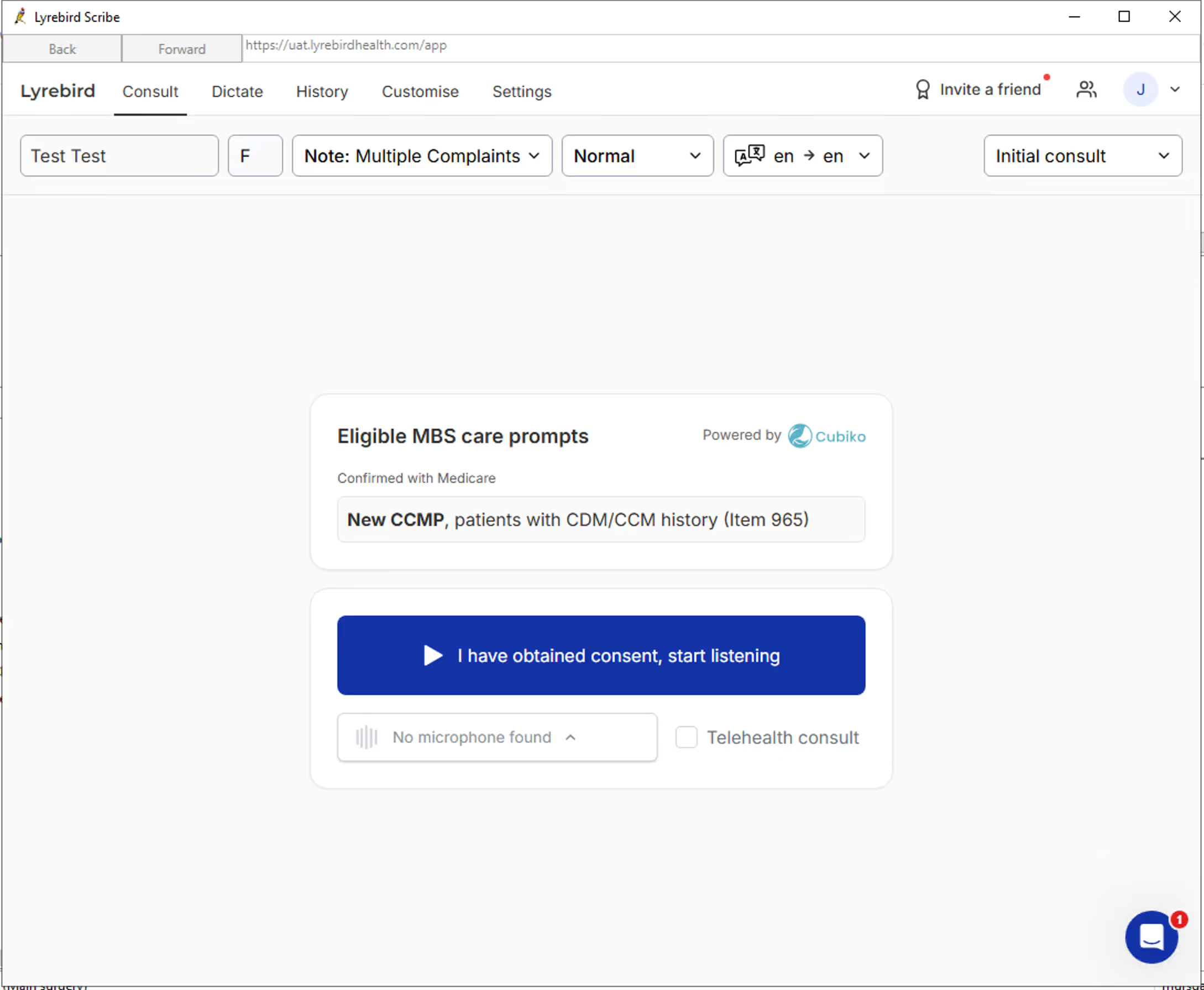
Lyrebird's integration with Cubiko flags eligible MBS items in real-time at the start of the consult. This acts as a real-time compliance check, protecting your quarterly BBPIP payment and ensuring the highest-value item is always claimed.
2. Increasing GP capacity to offset bulk-billing costs
Moving to a fully bulk-billed model (under BBPIP) reduces per-service revenue compared to private billing. To maintain or improve financial sustainability, GPs must increase service volume without increasing hours or sacrificing care quality.
How Lyrebird helps
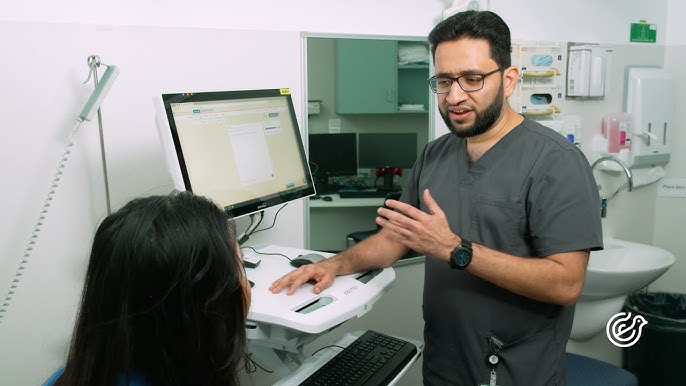
Lyrebird streamlines clinical documentation by capturing and structuring the consultation automatically. Dr. Georges Oteng, GP, The Family Practice, has seen a 30% increase in capacity after using Lyrebird. This saved time is converted directly into more available appointments, driving more services and therefore more BBI/BBPIP revenue, while significantly reducing the administrative burden that leads to GP burnout.
“Lyrebird has completely transformed my practice. I have increased my capacity by 30%, and I’m able to see more patients without staying at the clinic until 8pm.”
—Dr Georges Oteng, GP, The Family Practice
3. Streamlining complex and high-value MBS items
Administration-heavy services like Chronic Condition Management Plans (CCMP) and Mental Health Treatment Plans (MHTP) have tight profit margins due to the extensive manual documentation required.
How Lyrebird helps
Lyrebird’s smart workflows inside Bp Premier automate the generation of these documents. This means complex items like CCMPs (item 965) and initial MHTPs (item 2715) can be completed in up to 50% less time. The CCMP workflow, for example, allows a GP to complete the plan in under 20 minutes (compared to 40 minutes manually), helping to drive revenue and ensure patients receive detailed, high-quality plans.
4. Navigating the Better Access documentation changes
The new mental health rules remove dedicated review items and require GPs to use time-tiered general attendance items for reviews. This demands robust, clinically justified, time-based documentation to ensure Medicare compliance for the item billed (e.g., Level C vs D) and adherence to the 'usual medical practitioner' or MyMedicare continuity rules.
How Lyrebird helps
Lyrebird automatically generates comprehensive, structured notes that capture the depth and duration of the mental health consultation, providing clear justification for the time-tiered item billed. This not only makes the documentation process efficient but also creates an audit-proof record that supports the mandated requirements for continuity of care and accreditation.
Your action plan before November 1
The upcoming reforms represent a monumental opportunity for Australian General Practice. By expanding bulk billing incentives and introducing the BBPIP, the government is signalling a significant investment in practices committed to accessible care.
The challenge now is not just in understanding the changes, but in executing them flawlessly to ensure compliance and profitability. Practices that view this transition as a mandate for enhanced efficiency, supported by tools like Lyrebird, will be the ones that succeed in balancing the delivery of high-quality, high-volume care with financial sustainability.
- Educate and audit: Thoroughly review the official resources on the Expanded BBIs, the BBPIP, and the Better Access redesign to ensure every GP and staff member understands the new claiming and compliance rules.
- Invest in efficiency: Recognise that success under the new model requires maximising GP capacity and streamlining documentation.
- Contact Lyrebird: Book a time with us to see a personalised demonstration of how Lyrebird's workflows can be deployed in your clinic to ensure maximum BBPIP compliance, drive revenue, and safeguard your GPs from administrative burnout under the new Medicare rules.