A Guide To Writing Great SOAP Notes

Introduction
In the world of healthcare, effective communication and documentation are crucial for providing high-quality care. One widely adopted method of documentation is the Subjective, Objective, Assessment, and Plan (SOAP) note. SOAP notes provide a structured and organised way for healthcare providers to document patient information and track their progress. In this comprehensive guide, we will look at astep-by-step process of writing SOAP notes, discuss the legal and ethical aspects, and explore how technology is changing the note-taking process in medical note writing.
Section 1: Understanding SOAP
What are SOAP Notes?
SOAP notes are a systematic method of documenting patient encounters, capturing essential information, and facilitating effective communication between healthcare providers. The acronym SOAP represents the four sections of the note: Subjective, Objective, Assessment, and Plan. Each section serves a specific purpose in documenting the patient's condition, evaluation, and treatment plan.
The Importance of SOAP Notes
SOAP notes play a vital role in patient care and clinical decision-making. They provide a comprehensive record of the patient's health status, facilitate continuity of care between healthcare professionals, and serve as a legal and ethical documentation of the care provided. SOAP notes offer a cognitive framework for clinical reasoning and help guide healthcare workers in assessing, diagnosing, and treating patients.
Section 2: Step-by-Step Guide to Writing SOAP Notes
Step 1: Subjective - Gathering Information
The Subjective section of the SOAP note captures the patient's subjective experiences, personal views, and feelings. It provides context for the Assessment and Plan sections. To gather relevant information, healthcare providers should:
- Determine the chief complaint (CC) or presenting problem reported by the patient. This can be a symptom, condition, or previous diagnosis that describes why the patient is seeking care.
- Conduct a thorough history of present illness (HPI) by asking questions about the onset, location, duration, characterisation, alleviating and aggravating factors, radiation, temporal factors, and severity of the complaint.
- Gather information about the patient's medical history, surgical history, family history, and social history.
- Perform a review of systems (ROS) to uncover any additional symptoms not mentioned by the patient.
- Document current medications and allergies.
Step 2: Objective - Gathering Objective Data
The Objective section of the SOAP note focuses on the objective findings obtained during the patient encounter. This includes:
- Vital signs such as blood pressure, heart rate, respiratory rate, and temperature.
- Physical examination findings, including general appearance, specific organ systems, and any abnormal findings.
- Laboratory data, imaging results, and other diagnostic tests.
- Recognition and review of documentation by other clinicians.
Step 3: Assessment - Synthesising Information
In the Assessment section, healthcare providers synthesise the subjective and objective evidence to arrive at a diagnosis or list of possible diagnoses. This section includes:
- Listing the main problems or diagnoses in order of importance.
- Providing a differential diagnosis, which is a list of potential diagnoses ranked from most to least likely.
- Explaining the thought process and decision-making behind the differential diagnosis.
- Considering the possibility of other diagnoses that may harm the patient but are less likely.
Step 4: Plan - Developing the Treatment Plan
The Plan section outlines the next steps and treatment plan for the patient. It includes:
- Specifying any additional testing or consultations needed to address the patient's condition.
- Describing the therapy or medications required.
- Referring the patient to specialists or other healthcare professionals if necessary.
- Providing patient education and counselling.
- Setting short-term and long-term goals for the patient's treatment.
- Considering nutritional, physical, and medical factors that contribute to the therapeutic goals.
Section 3: Legal and Ethical Considerations
Legal Implications of SOAP Notes
SOAP notes serve as legal documentation of the care provided to patients. Accurate and comprehensive SOAP notes can protect healthcare providers in potential legal disputes by providing evidence of the care provided, the reasoning behind treatment decisions, and the patient's progress over time. However, it's essential to ensure that SOAP notes adhere to legal and ethical standards, including patient confidentiality and privacy.
Ethical Considerations in SOAP Notes
Ethical considerations in SOAP notes revolve around maintaining patient autonomy, beneficence, and non-maleficence. Healthcare providers should ensure that their notes accurately reflect the patient's subjective experiences, respect their values and preferences, and prioritise their well-being. It is important to obtain informed consent from patients regarding the use of their information for documentation purposes.
Section 4: Technological Advancements in Medical Note Taking
Evolution of SOAP Notes and Technology
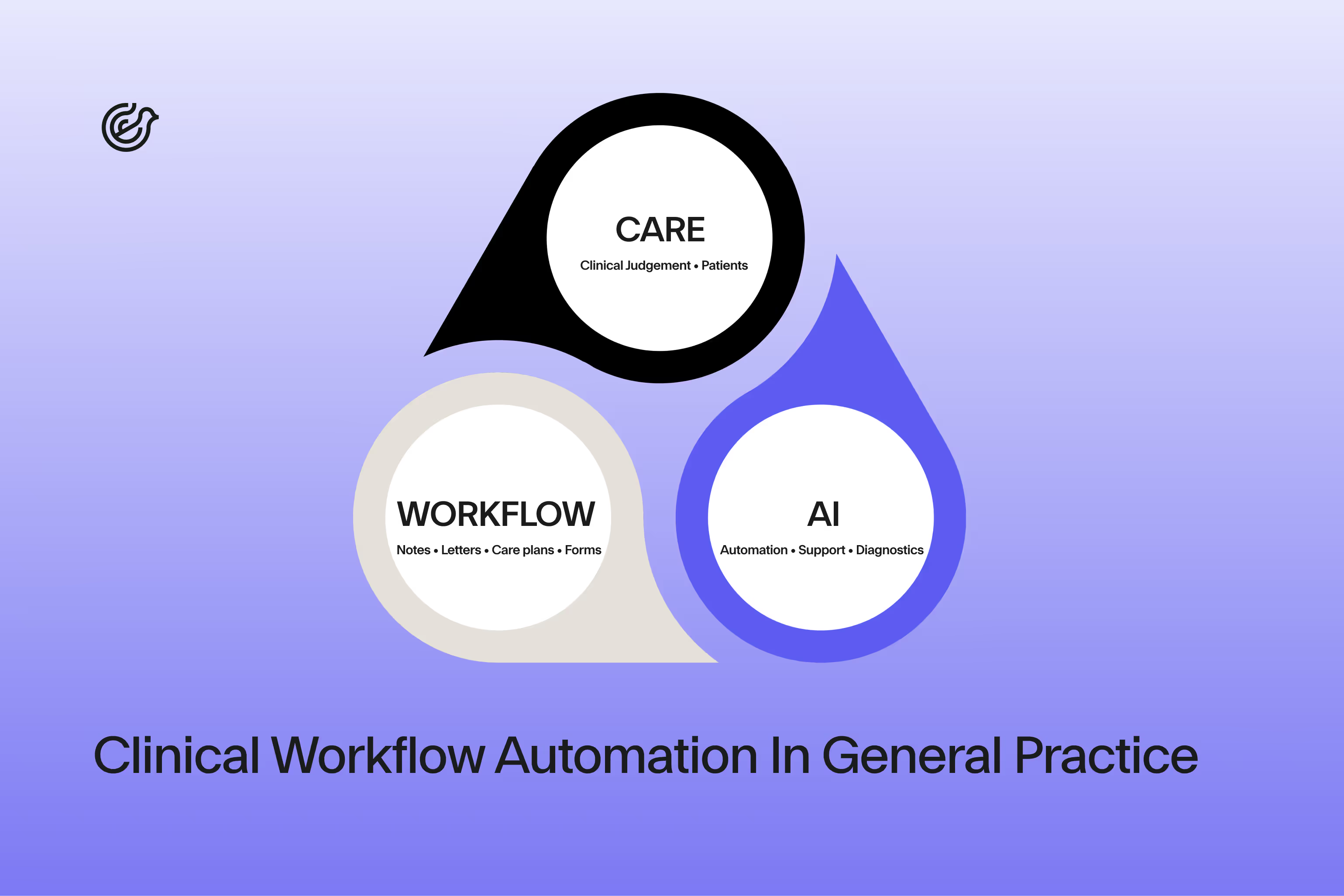
With advancements in technology, the process of taking and managing SOAP notes has become more efficient and streamlined. Electronic Health Records (EHRs) have replaced traditional paper-based documentation, allowing for easy access, retrieval, and sharing of patient information. Lyrebird Health, a software that automatically generates all of your relevant medical documentation allows you to focus on the patient rather than spending your day taking notes and writing letters. Learn more about Lyrebird here.
Benefits of Lyrebird Health
Using natural language processing algorithms, Lyrebird Health analyses patient encounter data and generates accurate and comprehensive medical documentation in real-time. This eliminates the need for manual note-taking and transcription, allowing clinicians to focus more on patient care.
Furthermore, Lyrebird Health's autogeneration capabilities ensure standardised and consistent documentation across healthcare providers, improving communication and collaboration among clinicians. By reducing the administrative burden and enhancing efficiency in medical documentation, Lyrebird Health empowers healthcare clinics to deliver high-quality patient care while optimising their operational processes.
Conclusion
SOAP notes are a fundamental tool for effective clinical documentation and communication in healthcare. By following a structured approach and incorporating technological advancements, healthcare providers can create comprehensive and accurate SOAP notes that support optimal patient care. As technology continues to evolve, the process of documenting SOAP notes will become more seamless and efficient, further enhancing the quality of care provided to patients.
Remember, accurate and detailed SOAP notes are essential for providing effective care, ensuring legal compliance, and promoting patient safety. By mastering the art of SOAP note documentation, healthcare providers can enhance their practice and contribute to improved patient outcomes.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Please consult with a qualified healthcare professional for specific medical concerns or questions.
References:
- Gogineni H, Aranda JP, Garavalia LS. Designing professional program instruction to align with students' cognitive processing. Curr Pharm Teach Learn. 2019 Feb;11(2):160-165.
- Andrus MR, McDonough SLK, Kelley KW, Stamm PL, McCoy EK, Lisenby KM, Whitley HP, Slater N, Carroll DG, Hester EK, Helmer AM, Jackson CW, Byrd DC. Development and Validation of a Rubric to Evaluate Diabetes SOAP Note Writing in APPE. Am J Pharm Educ. 2018 Nov;82(9):6725.
- Lisenby KM, Andrus MR, Jackson CW, Stevenson TL, Fan S, Gaillard P, Carroll DG. Ambulatory care preceptors' perceptions on SOAP note writing in advanced pharmacy practice experiences (APPEs). Curr Pharm Teach Learn. 2018 Dec;10(12):1574-1578.
- Sando KR, Skoy E, Bradley C, Frenzel J, Kirwin J, Urteaga E. Assessment of SOAP note evaluation tools in colleges and schools of pharmacy. Curr Pharm Teach Learn. 2017 Jul;9(4):576-584.
- Belden JL, Koopman RJ, Patil SJ, Lowrance NJ, Petroski GF, Smith JB. Dynamic Electronic Health Record Note Prototype: Seeing More by Showing Less. J Am Board Fam Med. 2017 Nov-Dec;30(6):691-700.
- Santiago LM, Neto I. SOAP Methodology in General Practice/Family Medicine Teaching in Practical Context. Acta Med Port. 2016 Dec 30;29(12):854-859.